In response to the coronavirus pandemic, the world has rushed to deploy infrared thermal imaging cameras (also known as infrared radiometers) to measure people’s temperature and the technology has become big business.
Since the pandemic began, thermal cameras have been deployed in areas of high-density foot traffic such as airports, shopping centres, nursing homes, factories, office buildings, schools, even hairdressers. This is raising questions about their safety and accuracy.
And while the accuracy of these devices depends on how they are used, we can say for certain that the technology poses no harm to people and is perfectly safe.
How do thermal cameras work?
Infrared thermal imaging cameras measure radiated energy from an object surface, such as the human skin, without any need to touch that surface. Different temperatures are shown as different colours on a thermogram, which can change colour, for example, at the threshold for a fever (38℃).
This idea goes back to 1800, when William Herschel, the Royal Astronomer, who was already famous for discovering the planet Uranus, first described the existence of infrared radiation. He passed sunlight through a glass prism and measured the temperature of each rainbow colour with different thermometers. He noticed a higher temperature in a dark area and called this “radiant heat”: we now call this infrared radiation.
Early thermal imagers became available around 1959 and were used initially to measure the increased heat over arthritic hips. Other medical applications have included Raynaud’s phenomenon (which affects blood circulation), diabetes symptoms and melanoma, however screening for fever has become its most common clinical use today.
In the past, fevers were diagnosed using mercury thermometers, which for safety reasons have been replaced by infrared devices that measure tympanic (ear drum) temperature. However, these require close contact with the person, which is not ideal in screening for potential cases of coronavirus.
Today’s infrared cameras are extremely reliable with very few moving parts, are simple to operate, but to be accurate it is vital the user targets the correct area of the face. In the 2009 Swine Flu pandemic, the forehead was the target area used, and this gave misleading results.
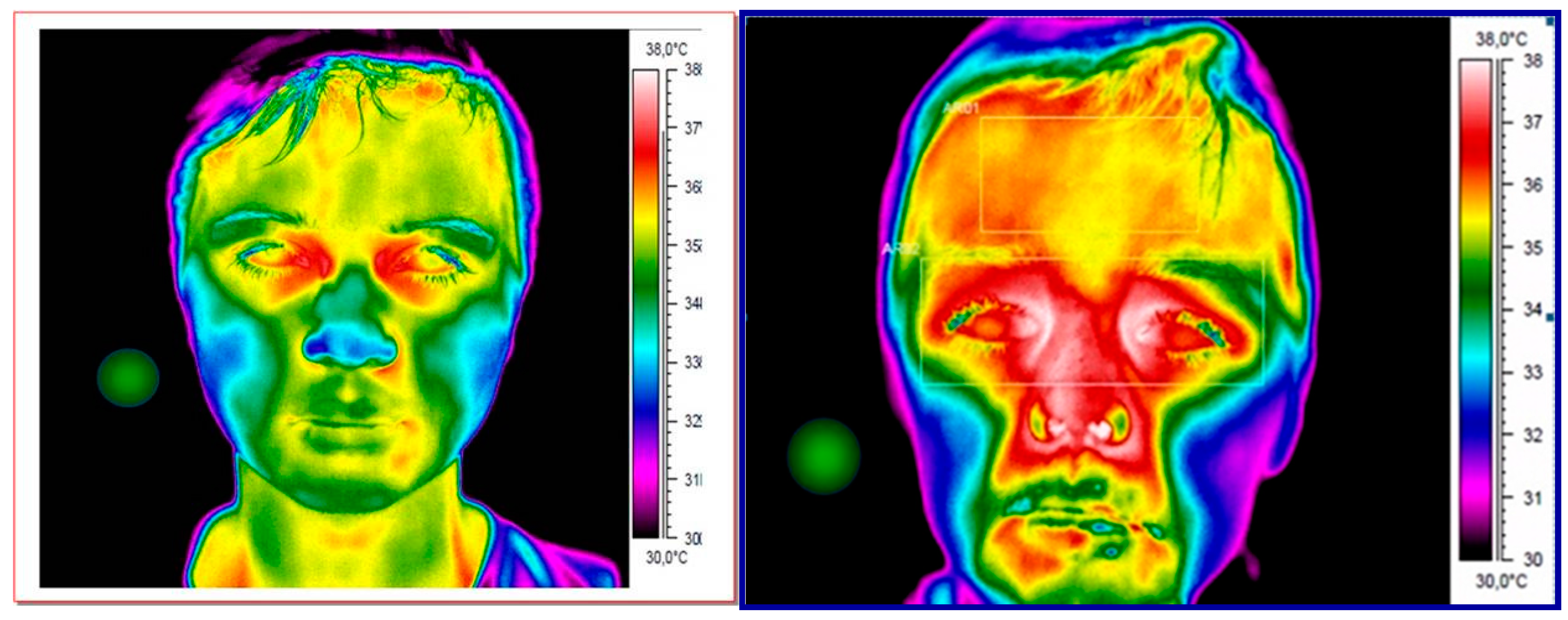
The latest update from the thermographs from the International Organization for Standardization confirms the region that gives the most stable results is near the inner canthi (tear duct) because it is located directly over a major artery. If this area is one or more degrees higher than the baseline average (37℃), there is a high probability that the person has a fever, which should then be verified in the usual way with a traditional infrared tympanic thermometer.
In the image below, we can see the difference between how a child without a fever (on the left) shows up on a thermal camera compared a child who has a fever (on the right), when the camera is targeted on the tear ducts.
The limitations of thermal cameras
Fever is an important sign of infection with COVID-19 but will not always be present. An infectious person in the early stages of the disease may have no symptoms at all, or they may have some symptoms but no fever.
This is why the Medicines and Healthcare products Regulatory Agency in the UK warned that temperature screening cannot be relied upon for detecting cases of COVID-19.
Still, there is clinical evidence to support the use of thermal cameras for fever screening. The reality is that with the right thermal imaging camera, the right lens and following the correct guidelines and standards, it can be effective as a screening tool.
How to get the best results
To maximise the chances of success, thermal cameras should be positioned close to and level with the eyes, to capture a cluster of image pixels from near the tear ducts.
The type of camera and lens is extremely important – an infrared radiometer with at least 320 x 240 pixels is considered a minimum requirement with a standard lens between 20-24°. Ideally, the face should occupy at least 75% of the image and so a distance between the person being scanned and the camera of 70-120cm is recommended to achieve this.
If these distances are extended, it will result in a drop in temperature. You can see the difference in temperature of the same person at 600cm results in a drop of 1.6℃.
Regular calibration of the camera and recording of the environmental temperature on the image is crucial, because variation in the room temperature and humidity will also affect the result. Draughts and direct sunlight can also cause difficulties and should be avoided.
Most important to know, for those who are worried about safety, is that infrared cameras, like any other cameras, capture energy emitted from the body and do not generate any radiation themselves. So there is no risk from them.
However, although proper and careful use will minimise false negative and positive results, these problems will occur, and so it is important that the limitations of this technology for screening are understood and it is used in conjunction with other measures to limit the spread of coronavirus. If deployed alongside social distancing, mask wearing and hand washing, thermal cameras can still be part of our arsenal in the fight to control this disease.



 Nintendo Shares Slide After Earnings Miss Raises Switch 2 Margin Concerns
Nintendo Shares Slide After Earnings Miss Raises Switch 2 Margin Concerns  SoftBank Shares Slide After Arm Earnings Miss Fuels Tech Stock Sell-Off
SoftBank Shares Slide After Arm Earnings Miss Fuels Tech Stock Sell-Off  SpaceX Prioritizes Moon Mission Before Mars as Starship Development Accelerates
SpaceX Prioritizes Moon Mission Before Mars as Starship Development Accelerates  Oracle Plans $45–$50 Billion Funding Push in 2026 to Expand Cloud and AI Infrastructure
Oracle Plans $45–$50 Billion Funding Push in 2026 to Expand Cloud and AI Infrastructure  Nvidia Nears $20 Billion OpenAI Investment as AI Funding Race Intensifies
Nvidia Nears $20 Billion OpenAI Investment as AI Funding Race Intensifies  Instagram Outage Disrupts Thousands of U.S. Users
Instagram Outage Disrupts Thousands of U.S. Users  Sony Q3 Profit Jumps on Gaming and Image Sensors, Full-Year Outlook Raised
Sony Q3 Profit Jumps on Gaming and Image Sensors, Full-Year Outlook Raised  Palantir Stock Jumps After Strong Q4 Earnings Beat and Upbeat 2026 Revenue Forecast
Palantir Stock Jumps After Strong Q4 Earnings Beat and Upbeat 2026 Revenue Forecast  SoftBank and Intel Partner to Develop Next-Generation Memory Chips for AI Data Centers
SoftBank and Intel Partner to Develop Next-Generation Memory Chips for AI Data Centers  Google Cloud and Liberty Global Forge Strategic AI Partnership to Transform European Telecom Services
Google Cloud and Liberty Global Forge Strategic AI Partnership to Transform European Telecom Services  Elon Musk’s SpaceX Acquires xAI in Historic Deal Uniting Space and Artificial Intelligence
Elon Musk’s SpaceX Acquires xAI in Historic Deal Uniting Space and Artificial Intelligence  AMD Shares Slide Despite Earnings Beat as Cautious Revenue Outlook Weighs on Stock
AMD Shares Slide Despite Earnings Beat as Cautious Revenue Outlook Weighs on Stock  Tencent Shares Slide After WeChat Restricts YuanBao AI Promotional Links
Tencent Shares Slide After WeChat Restricts YuanBao AI Promotional Links  Nvidia Confirms Major OpenAI Investment Amid AI Funding Race
Nvidia Confirms Major OpenAI Investment Amid AI Funding Race  Sam Altman Reaffirms OpenAI’s Long-Term Commitment to NVIDIA Amid Chip Report
Sam Altman Reaffirms OpenAI’s Long-Term Commitment to NVIDIA Amid Chip Report  Nvidia, ByteDance, and the U.S.-China AI Chip Standoff Over H200 Exports
Nvidia, ByteDance, and the U.S.-China AI Chip Standoff Over H200 Exports