Tuberculosis (TB) is a lung disease caused by the bacterium Mycobacterium tuberculosis. It’s transmitted through air droplets when an infectious person coughs or sneezes. The disease can be treated, but it’s a long process with the drugs that are currently available. It remains a major health problem: globally, about 1.6 million died from it in 2017.
Most of these deaths occurred in the developing world. The African continent has a particularly severe TB burden. This is worsened by the emergence of multidrug-resistant TB; patients with this form of the disease respond poorly to the usual first-line drugs. TB and HIV co-infection is also a big problem.
There are some glimmers of hope. Globally, TB related deaths dropped by 33% between 2000 and 2017. There’s also a new push from the World Health Organisation (WHO) to reduce new TB cases by 90% by 2035. But for this to happen, new therapies and diagnostic tools are needed.
There are some promising therapies in the pipeline, particularly when it comes to host-directed therapies and biomarkers. The first refers to drugs that strengthen the immune system and reduce lung damage. Biomarkers are blood- or tissue-based indicators that tell clinicians about the presence of latent (or dormant) TB, the development of active TB and its progression.
Governments, global funding agencies, national research councils and the private sector now need to invest resources in developing these therapies to the point where they can be used widely. This is crucial if the WHO’s ambitious targets are to be met.
Host-directed therapies
In TB treatment, host-directed therapies have two major goals. One is to stimulate key components of the immune system to control TB infection. The other involves limiting damage to the lung tissue in a bid to slow down TB’s progression.
Host-directed therapies can also be combined with standard treatment regimens. This will likely shorten the current course of TB treatment, which at its shortest lasts for about six months.
Some of the host-directed therapies that are currently being investigated include:
-
Vitamin D, which induces specific immune molecules that have protective effects against the TB bacteria.
-
Non-steroidal anti-inflammatory drugs (ibuprofen, zileuton and aspirin). These work by suppressing excessive inflammation and tissue pathology and reduce bacterial burdens in the lung.
-
Statins reduce cholesterol levels and limit bacterial growth in the body’s immune cells.
-
Angiogenesis inhibitor (Bevacizimub) is a drug that works by blocking formation of new blood vessels (neovascularisation) in lung granulomas (small areas of inflammation). It might improve anti-TB drug penetration into granulomas and increase air supply.
Diagnostics and biomarkers
Treating TB is only one part of the puzzle. Proper, timely diagnosis and a good understanding of the disease’s progression in an individual patient are also important.
The disease is currently diagnosed in several ways. These include viewing a sputum sample under a microscope; through a skin test; or through a blood test.
But biomarkers could hold useful answers, too. About one-third of the world’s population is infected with the bacterium that causes TB. Between 5% and 10% of these latently infected individuals will develop the active disease in their lifetime. Biomarkers could be used to reliably predict who these individuals are. The individuals could then be treated preemptively.
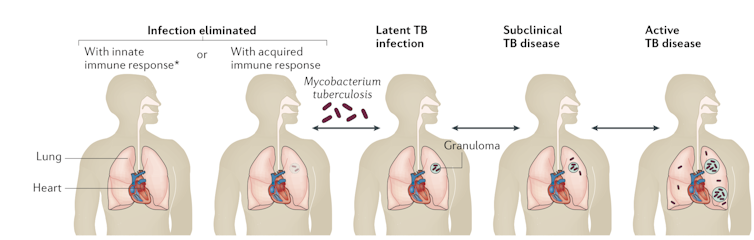
A representation different stages of TB. author supplied
There have been exciting studies along these lines. These have identified the gene and protein signatures associated with the sub-clinical stage of TB – that is, latently infected individuals on the brink of converting to active TB. Such signatures are evident in patients’ blood as early as 200 days before the onset of active TB.
Metabolic biomarkers associated with the pre-symptomatic stage of TB have also been identified. Again, these are detectable before the onset of the active disease.
However, the pipeline for biomarkers that can detect other forms of TB, among them the drug-resistant variety, is weak. More work remains to be done in this area.
Investment needed
Studies like these, and others, require increased investments from a number of funders. These are crucial if scientists are to take their findings into the clinical trial stages and eventually develop tools that can be used in everyday TB diagnosis and treatment.
This is imperative if the world is to end TB.
Sephekana Samuel Mohapi, a Master’s student in the University of Cape Town’s Department of Pathology, contributed to this article.



 Neuralink Expands Brain Implant Trials with 12 Global Patients
Neuralink Expands Brain Implant Trials with 12 Global Patients  SpaceX Starship Test Flight Reaches New Heights but Ends in Setback
SpaceX Starship Test Flight Reaches New Heights but Ends in Setback  JPMorgan Lifts Gold Price Forecast to $6,300 by End-2026 on Strong Central Bank and Investor Demand
JPMorgan Lifts Gold Price Forecast to $6,300 by End-2026 on Strong Central Bank and Investor Demand  NASA Faces Major Workforce Reduction as 20% of Employees Prepare to Leave
NASA Faces Major Workforce Reduction as 20% of Employees Prepare to Leave  Neuren Pharmaceuticals Surges on U.S. Patent Win for Rare Disorder Drug
Neuren Pharmaceuticals Surges on U.S. Patent Win for Rare Disorder Drug  Blue Origin’s New Glenn Achieves Breakthrough Success With First NASA Mission
Blue Origin’s New Glenn Achieves Breakthrough Success With First NASA Mission  Nasdaq Proposes Fast-Track Rule to Accelerate Index Inclusion for Major New Listings
Nasdaq Proposes Fast-Track Rule to Accelerate Index Inclusion for Major New Listings  FDA Adds Fatal Risk Warning to J&J and Legend Biotech’s Carvykti Cancer Therapy
FDA Adds Fatal Risk Warning to J&J and Legend Biotech’s Carvykti Cancer Therapy 































